Continuous Vs Discontinuous Therapy With Penicillin

Stability Studies of 16 Antibiotics for Continuous Infusion in Intensive Care Units and for Performing Outpatient Parenteral Antimicrobial Therapy
1
Pharmacy Department, University Hospital, 54511 Vandoeuvre-lès-Nancy, France
2
Infostab, Non-Profit Association, 54180 Heillecourt, France
3
EA 4360 APEMAC, Lorraine University, 54000 Nancy, France
4
Infectious Diseases Department in Charge of Mobile Infectiology Team University Hospital, 54511 Vandoeuvre-lès-Nancy, France
*
Author to whom correspondence should be addressed.
Academic Editor: Jeffrey Lipman
Received: 9 March 2022 / Revised: 24 March 2022 / Accepted: 26 March 2022 / Published: 29 March 2022
Abstract
The use of continuous infusion to improve the therapeutic efficacy of time-dependent antibiotics has been demonstrated. There is still a lack of data to safely perform these continuous infusions. The objectives in this study were to evaluate the stability by using stability-indicating methods (High-Performance Liquid Chromatography) of 16 antibiotics in concentrated solutions, especially for administration in intensive care units and solutions in elastomeric diffusers at 37 °C for outpatient parenteral antimicrobial therapy. The solutions were considered stable if the percentage of the drug was ≥90%, and the colour and clearness remained unchanged. In syringes, the stability data vary from 4 to 8 h (h) for meropenem in Dextrose 5% (D5W) and Normal Saline (NS), respectively, 6 h for cefotaxime, 12 h for cefoxitin, and 24 h for aztreonam, cefazolin, cefepime, cefiderocol, ceftazidime/avibactam, ceftolozane/tazobactam in NS and D5W, and in water for injection for cloxacillin. A stability period of 48 h has been validated for vancomycin (D5W), aztreonam, and piperacillin/tazobactam. Cefoxitin, cefazolin, cefepime, cefotaxime, cloxacillin, and piperacillin are unstable for diffuser administration. In diffusers, stability times vary from 6 h for cefiderocol, 8 h for ceftazidime, 12 h for ceftazidime/avibactam and ceftolozane/tazobactam (NS), 24 h for temocillin (NS) and piperacillin/tazobactam (D5W), up to 48 h for aztreonam and vancomycin. Solutions stored at 37 °C are less stable and allow the administration of seven antibiotics using diffusers.
1. Introduction
The value of continuous infusion for time-dependent antibiotics has been demonstrated for several years. In particular, for beta-lactam antibiotics, therapeutic optimisation via continuous infusion makes it possible to target a free plasma concentration of beta-lactam antibiotics between 4 and 8 times the Minimum Inhibitory Concentration (MIC) of the incriminated bacteria, and thus to obtain a maximum rate of bactericidia [1]. A meta-analysis including 13 randomised controlled trials evaluating the impact of continuous or discontinuous beta-lactam administration in critical care patients showed improved clinical recovery in septic patients and patients at high risk of mortality, as well as in patients treated with continuous infusion [2]. The use of continuous infusion is also recommended in cases of high MIC of the causative bacteria or critical care patients with non-fermenting Gram-negative bacilli (A. baumanii and P. aeruginosa) to improve the clinical cure rate [3,4]. For vancomycin, a meta-analysis demonstrated that continuous infusion compared to intermittent administration is associated with a 53% reduction in the risk of acute kidney injury without influencing overall mortality [5].
The use of antibiotic infusions in critical care is frequent. A large European multicentre study reported the use of antibiotics in 64% of patients during their hospitalisation in an intensive care unit (ICU) [6]. In these ICUs, under real-life conditions, antibiotic infusions are often carried out in small volumes at high concentrations. The question then arises of the stability of these high-concentration solutions over a long period of time to achieve these continuous infusions.
Upon discharge from the hospital, patients can continue treatment with Outpatient Parenteral Antimicrobial Therapy (OPAT). The major benefits of OPAT are the reduction or avoidance of hospital stays, the reduction in nosocomial infections and hospital-related conditions, significant cost savings, and improved quality of life for the patient [7,8]. The use of continuous home infusion may be recommended for infections where the risk of failure is high, for infections with high MIC bacteria, or for infections where the delivery of beta-lactams is difficult, such as foreign-material infections [9,10,11]. Portable elastomeric devices allow these continuous infusions to be performed in the patient's home. Information provided by pharmaceutical companies in the Summaries of Products Characteristics (SmPC) does not provide details for continuous intravenous administration of highly concentrated solutions for administration in syringes in ICUs or for solutions at an elevated temperature (32 or 37 °C) in elastomeric devices for continuous infusion at home (OPAT) [12].
It is, therefore, crucial to carry out stability studies to safely perform these continuous infusions. As specified in the ASEAN guidelines (2005), the stability of an active ingredient or a pharmaceutical speciality is its ability to maintain its properties within specific limits throughout its lifetime. The chemical, physical, microbiological, and biopharmaceutical aspects of stability must be considered [13]. Drug solutions are usually considered chemically stable if they retain their chemical characteristics: The percentage of the drug intact remains above 90% of the initial concentration [14]. The stabilities of injectable antibiotics have been published, but often at too-low concentrations, which do not allow a small volume for the preparation of syringes for continuous administration over 12 or 24 h or have not been studied at body temperature for administration at home using elastomeric diffusers [15].
The aim of this study was to determine the physicochemical stability of 16 antibiotics, namely amoxicillin, aztreonam, cefazolin, cefepime, cefiderocol, cefotaxime, cefoxitin, ceftazidime, ceftazidime/avibactam, ceftolozane/tazobactam, cloxacillin, meropenem, piperacillin, piperacillin/tazobactam, temocillin, and vancomycin, under two conditions for continuous infusion. The first condition is in a high-dose polypropylene syringe at 20–25 °C for ICUs. The second condition is at 37 °C in portable elastomeric devices for OPAT. Only amoxicillin was packaged in polyolefin bags for administration using a volumetric pump and stored at room temperature [16].
To study the physico-chemical stability of a drug, a determination of the active ingredient must be carried out using a separative analytical method, in order to be able to separate the active substance from its degradation products. To perform these stability studies, we used High-Performance Liquid Chromatography (HPLC) [17].
2. Results
2.1. Chemical Stability by HPLC
The pre-study made it possible to eliminate certain antibiotics due to the appearance of a precipitate after storage at 37 °C (cefazolin, cloxacillin) or a change in the colour of the solution (cefotaxime, cefoxitin, and piperacillin).
The validation method criteria for HPLC analysis are presented in Table 1. Linearity was demonstrated for all molecules, with an R2 value between [0.9981 and 0.9999]. The calibration curves agreed with the linear model via a non-linearity test ANOVA (Fexp < Fth = 3.71) for all molecules. The homogeneity of the variances was also proven by a Cochran test (Cexp < Cth = 0.684) for all molecules. Intraday and interday precisions were less than 2.5%. The analytical methods were stability-indicating.
Table 2 presents the concentrations of antibiotics in polypropylene syringes and Table 3 presents the concentrations in elastomeric containers. The concentrations of amoxicillin obtained in polyolefin bags are presented in Table 2. Several examples of chromatograms obtained after reconstitution (T0 h) are presented in Figure 1.
2.2. The pH Measurement
pH value variations were less than one pH unit except for 125 mg/mL cefazolin in both solvents in syringes (6 g in 48 mL) after 48 h, 125 mg/mL cefoxitin in NS after 12 h, and piperacillin/tazobactam 16 g/0.75 g in NS in 240 mL in an elastomeric container after 24 h.
2.3. The Visual and Subvisual Evaluation
During the stability study, several physical changes were observed, with a major intensification of yellowing for solutions whose chemical stability specifications were maintained. After 12 h, cefotaxime solutions at 83.3 and 125 mg/mL in syringes and ceftolozane/tazobactam at 25/12.5 mg/mL in diffusers after 24 h presented visual modifications. These physical changes were observed in both NS and D5W.
The particle counter test was not available at the beginning of the stability studies and was carried out on new syringes at the end of the studies by measuring the number of particles inferior to 10 µm and 25 µm according to European Pharmacopoeia. This test was only performed on antibiotics that were visually and chemically stable. All samples were within the specifications of European Pharmacopoeia.
3. Discussion
3.1. Choice of the Temperature
When administered at home, the elastomeric container is placed under the clothes near the body. The temperature of the solution is higher than the classical ambient temperature at 25 °C and is near body temperature. Some authors or guidelines suggest using 32 °C for these stability studies considering that the device is not in the body and that the temperature is lower [18]. Other teams work by using body temperature, considering the worst condition that can be met in some hot countries depending on geographical area. In our studies, we decided to use the latter conditions.
3.2. Choice of Molecules and Study Design
Certain time-dependent antibiotics were not studied in our stability studies, such as ceftriaxone or ertapenem, because of their long half-life requiring only one injection per day. Conversely, molecules with well-defined instability, such as imipenem/cilastatin (stable for 4 h at a concentration of 5 mg/mL), were not studied [19], as well as meropenem in a diffuser. The study of temocillin in syringes was not performed as the laboratory had already provided these stability data in NS and D5W [20]. Amoxicillin was studied at 20 mg/mL in polyolefin bags to validate data of the literature review of Diamantis et al. [17]. Stability up to 12 h has been demonstrated, allowing two infusions per day by a volumetric pump (4 g/200 mL or 6 g/300 mL, for example).
3.3. About the Solvents Used
NS and D5W were used for all the products except cloxacillin, where SWFI was used. Stability can be different according to the solvent, depending on the pH value (D5W has a pH around 4 and NS around 6–7) or the chloride ions present in NS. Some products are not stable in both solvents. The choice of the solvent should be respected in accordance with stability studies. For the solution of cloxacillin at 250 mg/mL, the solvent used must be SWFI (12 g in 48 mL) and not NS or D5W due to precipitation. The osmolality of the solution is approximately 550 mOsmol/L, which allows intravenous administration [21]. We were able to validate the reconstitution of cloxacillin powder with only 3 mL of SWFI, allowing only one syringe of 12 g of cloxacillin to be made in 48 mL.
3.4. Limiting Factors
Due to poor solubility of piperacillin/tazobactam parenteral injection powder, higher concentrations could not be studied in syringes, as 12 g in 48 mL requires extensive shaking and ultrasonication to ensure complete dissolution, which was not feasible in ICUs.
According to the manufacturer's recommendations, a 1 g vial of cefiderocol should be reconstituted with 10 mL of solvent, which limits us to making a 48 mL syringe. Due to its high cost, the reduction of the reconstitution volume was not studied, which made it impossible to manufacture a 125 mg/mL (6 g/48 mL) syringe [22].
3.5. Citrated Buffered Solutions
An interesting approach to enhance the stability of very unstable drugs is to buffer the solution near pH 7 by using a citrated buffered solution. British teams used infusion bags of 0.3% sodium citrate in NS to study the stability of meropenem, piperacillin/tazobactam, and flucloxacillin. For 10 and 50 mg/mL flucloxacillin solutions, they demonstrated stability for 13 days stored at 2–8 °C followed by 24 h at 32 °C in two elastomeric containers (Accufuser and INfusor LV) [15]. In comparison, unbuffered flucloxacillin solutions lost up to 60% after storage at 37 °C for 24 h [23].
For piperacillin/tazobactam, extended stability was demonstrated with up to 13 days 2–8 °C plus 24 h at 32 °C "in-use" when using FOLFusor LV10 (Baxter) or Easypump II (B. Braun) pump devices [18]. However, these results were not observed for meropenem at concentrations between 6.25 mg/mL and 25 mg/mL, which was not sufficiently stable to administer as a 24-h infusion in ambulatory device reservoirs [24].
An Australian team studied the stability of benzylpenicillin and flucloxacillin after reconstitution with 4% sodium citrate and dilution in NS infusion bags. This approach was chosen because citrated infusion bags were not available on the Australian market.
Benzylpenicillin (15 and 60 mg/mL) and flucloxacillin (5 and 60 mg/mL) infusions in LV Elastomeric Infusor devices and 0.9% sodium chloride Viaflex bags were prepared as buffered and unbuffered solutions. Buffering was achieved by reconstituting antibiotic vials with sodium citrate 4%. Infusions were stored at 2–8 °C for 6 days then 37 °C for 24 h. Buffered benzylpenicillin 15 and 60 mg/mL and flucloxacillin 5 and 60 mg/mL in LV Elastomeric Infusors and 0.9% sodium chloride Viaflex bags appear chemically stable for 6 days refrigerated, as well as for a subsequent 24 h at 37 °C. Unbuffered solutions, prepared in NS, presented high instability. After 6 days at 2–8 °C and 1 day at 37 °C the concentration of 60 mg/mL benzylpenicillin in LV Infusor was 42.9% of the initial concentration instead of 100.3% for the buffered solution. Under the same storage conditions, the percentages of the initial concentration for 60 mg/mL flucloxacillin solutions were 63.1 and 99.6 [25]. These results showed the great potential of using citrated buffered solutions for molecules unstable in NS or D5W. However, this approach should be validated by a stability study for each molecule.
This is, to our knowledge, the first study to summarize the stability of 16 antibiotics, evaluated with the same robust methodology. It aimed to provide clinicians with a practical document to refer to when they want to optimize their treatment on a PK/PD level or to facilitate OPAT.
4. Materials and Methods
4.1. Chemical, Reagents and Products Used
The products used for the preparation of the mobile phase and the validation of the analytical method were of HPLC grade. Water for chromatography was obtained from a reverse-osmosis system (Millipore Iberica, Madrid, Spain), with a resistivity <15 MΩ cm. The antibiotic drugs used for the preparation of the tested solutions are summarized in Table 4. Normal saline (NS), sterile water for injection (SWFI), and 5% dextrose (D5W) used for the reconstitution of vials or the dilution of drugs were purchased from polyolefin bags (Easyflex, Macopharma, France) or glass vials (Chaix et du Marais, Lavoisier, France). For the preparation of solution tests, drugs were stored in polypropylene syringes (BD Plastipak 50 mL), in polyisoprene elastomeric devices (Baxter FOLFusor 5 mL/h or 10 mL/h), or in polyolefin bags (amoxicillin: Easyflex, Macopharma, Mouvaux, France).
4.2. Apparatuses
The following apparatuses were used for the stability studies:
- –
-
The High-Performance Liquid Chromatography (HPLC) system consisted of an ELITE LaChromVWR/ Hitachi plus autosampler, a VWR photodiode array detector L- 2455, and a VWR L-2130 HPLC pump. Data were acquired and integrated using EZChrom Elite (VWR, Agilent).
- –
-
pH meter (Bioblock Scientific model 93313).
- –
-
PAMAS particle counter, Rutesheim, Germany.
4.3. Methods
Considering the preparation of test solutions and storage, the choice of concentrations, solvents, and analysis times was based on a collegial decision between an infectious disease specialist and a pharmacist in relation to observed practices. Syringe preparations were performed at qs 48 mL and qs 120 or 240 mL in elastomeric devices. Each preparation corresponded to the total daily dose to be administered. The preparations of solutions tested are presented in Table 5.
Syringes and polyolefin bags (amoxicillin) were stored at room temperature, without protection from light and elastomeric devices at 37 °C in a climatic chamber. The stabilities of the antibiotics were studied at different analysis times over 48 h. For each condition, three syringes/bags or three elastomeric devices were prepared, and three samples for each preparation were chemically analysed.
To avoid time-consuming chemical stability studies by HPLC, a pre-study in glass vials was carried out at 37 °C at the concentrations used in elastomeric containers. The objective was to evaluate the physical stability by searching for the formation of precipitate or a change in colour to eliminate unstable drugs. If a physical modification was observed, this was concluded as physical instability, and the study of the chemical stability in diffusers was not carried out.
4.4. Chemical Stability by HPLC
Antibiotics solutions were analysed by stability-indicating reversed-phase HPLC methods adapted from previous publications.
The analytical conditions used for HPLC analysis (composition of the mobile phase, pH, flow rate, injection volume, wavelength for detection, retention time, and reference of the publication used for the choice of the method) are presented in Table 6.
Separation was performed on a LichroCART Merck C18 analytical column (5 µm, 125 mm × 4.0 mm) for all methods except ceftazidime, where a LichroCART Merck C18 column (5 µm, 250 mm × 5.0 mm) was used.
For four analytical methods (cefiderocol, cefotaxime, ceftazidime/avibactam, and piperacillin/tazobactam), a gradient elution mode was used.
Chemical stability was defined as no less than 90% of the initial concentration in relation to the evolution of potential degradation products [14].
4.5. Validation of the Analytical Methods
The validation of analytical methods was performed as recommended by the International Conference on Harmonisation Q2R1 (ICH) [40]. The calibration curves were constructed from the plots of peak area versus concentration. The linearity of each method was evaluated with 5 concentrations. For all calibration curves, the homogeneity of the variances was evaluated with a Cochran test of which the significance level was set at p < 0.05. An analysis of variance (ANOVA) of the linear regression data was performed to assess the significance (p < 0.05) of the proposed methods. Intra-day reproducibility and inter-day precision were evaluated. The limit of detection (LOD) was determined graphically for each analytical method. Selectivity and specificity were evaluated by forced degradation studies. For each analytical method, acid, basic, thermic, photolytic, and oxidative degradation were performed. The objective was to obtain a degradation between 10 and 20% of our molecules of interest to prove our methods are stability-indicating [17].
4.6. Physical Stability
Physical stability was defined as the absence of particulate, haze formation, or a colour change. The samples were visually inspected against a white/black background with the unaided eye at each analysis timepoint. Physical stability was also assessed by performing a particulate contamination test (PAMAS SVSS) at the beginning and the end of the study. The results were analysed according to the criteria of the European Pharmacopoeia [41,42].
4.7. pH Measurements
pH was measured at each time of analysis. A variation of more than one pH unit was considered unacceptable.
4.8. Summary of the Results
A summary of the results, including the physical and chemical stability usable in daily practice, is presented in Table 7.
5. Conclusions
Among the sixteen antibiotics tested at elevated concentrations, one was stable in polypropylene syringes for only 4 h (meropenem in D5W), one for 6 h (cefotaxime in D5W and NS), two for 8 h (ceftazidime (D5W) and meropenem (NS)), one for 12 h (cefoxitin in D5W), seven for 24 h (cefazolin, cefepime, cefiderocol, ceftazidime/avibactam in NS and D5W, ceftazidime and piperacillin in NS, cloxacillin (SWFI) at 250 mg/mL and 125 mg/mL in NS and D5W), and five were stable for 48 h (aztreonam, ceftolozane/tazobactam, piperacillin/tazobactam in NS and D5W, piperacillin and vancomycin in D5W). In elastomeric containers stored at 37 °C, we demonstrated 6 h stability for cefiderocol (NS and D5W), 8 h stability for ceftazidime (NS and D5W), ceftolozane/tazobactam (D5W), and piperacillin/tazobactam (in NS), 12 h stability for ceftolozane/tazobactam and ceftazidime/avibactam in NS, 24 h stability for piperacillin/tazobactam in D5W and temocillin (NS), and 48 h stability for aztreonam and vancomycin (NS and D5W). Amoxicillin (NS) in a polyolefin bag was stable for 12 h.
Clinicians must be aware that stability in syringes does not mean stability in diffusers. The choice of solvent must also be respected in accordance with these stability studies due to notable differences between NS, D5W, and SWFI. The concentration of the antibiotics studied must also be respected. It is possible to modify the dose/volume. Amoxicillin stability has been demonstrated at 20 mg/mL in bags for 12 h at room temperature. These new data allow us to perform administration for 12 h at 2 g/100 mL or at 4 g/200 mL, 5 g/250 mL, or 6 g/300 mL, for example. Regarding the diffusers, solutions must be protected from light by being worn under the patient's clothes, for example, or by a suitable device.
To our knowledge, this is the first study to summarize the stability data of 16 antibiotics at dosages relevant for use in clinical practice, evaluated with the same robust methodology. These new stability data allow for improved drug therapy and safer administration of these continuous infusions. The intention is to provide clinicians with a practical document to refer to when they want to optimize their treatment in terms of PK/PD or to facilitate OPAT.
Author Contributions
Conceptualization: A.C.; project administration: B.D.; conducting stability studies: G.L., E.D., Y.-E.N., B.B., C.P., G.A., and M.S.; writing: G.L. and E.D.; review and editing: A.C., E.D., and J.V.; supervision: E.D. and J.V. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
Thank you to Franck Blaise, Nathalie Sobalak, and Hubert Zénier for their help and involvement throughout this stability study. Thank you to Jacques Kuhnlé for reading through the manuscript and making corrections.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Mouton, J.W.; Punt, N.; Vinks, A.A. Concentration-Effect Relationship of Ceftazidime Explains Why the Time above the MIC Is 40 Percent for a Static Effect In Vivo. Antimicrob. Agents Chemother. 2007, 51, 3449–3451. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lee, Y.R.; Miller, P.D.; Alzghari, S.K.; Blanco, D.D.; Hager, J.D.; Kuntz, K.S. Continuous Infusion Versus Intermittent Bolus of Beta-Lactams in Critically Ill Patients with Respiratory Infections: A Systematic Review and Meta-Analysis. Eur. J. Drug Metab. Pharmacokinet. 2018, 43, 155–170. [Google Scholar] [CrossRef]
- De Jongh, R.; Hens, R.; Basma, V.; Mouton, J.W.; Tulkens, P.M.; Carryn, S. Continuous versus Intermittent Infusion of Temocillin, a Directed Spectrum Penicillin for Intensive Care Patients with Nosocomial Pneumonia: Stability, Compatibility, Population Pharmacokinetic Studies and Breakpoint Selection. J. Antimicrob. Chemother. 2008, 61, 382–388. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Roberts, J.A.; Abdul-Aziz, M.-H.; Davis, J.S.; Dulhunty, J.M.; Cotta, M.O.; Myburgh, J.; Bellomo, R.; Lipman, J. Continuous versus Intermittent β-Lactam Infusion in Severe Sepsis. A Meta-Analysis of Individual Patient Data from Randomized Trials. Am. J. Respir. Crit. Care Med. 2016, 194, 681–691. [Google Scholar] [CrossRef]
- Flannery, A.; Bissell, B.; Thompson Bastin, M.; Morris, P.; Neyra, J. Continuous versus Intermittent Infusion of Vancomycin and the Risk of Acute Kidney Injury in Critically Ill Adults: A Systematic Review and Meta-Analysis. Crit Care Med. 2020, 48, 912–918. [Google Scholar] [CrossRef] [PubMed]
- Vincent, J.-L.; Sakr, Y.; Sprung, C.L.; Ranieri, V.M.; Reinhart, K.; Gerlach, H.; Moreno, R.; Carlet, J.; Le Gall, J.-R.; Payen, D.; et al. Sepsis in European Intensive Care Units: Results of the SOAP Study. Crit. Care Med. 2006, 34, 344–353. [Google Scholar] [CrossRef] [PubMed]
- Norris, A.H.; Shrestha, N.K.; Allison, G.M.; Keller, S.C.; Bhavan, K.P.; Zurlo, J.J.; Hersh, A.L.; Gorski, L.A.; Bosso, J.A.; Rathore, M.H.; et al. 2018 Infectious Diseases Society of America Clinical Practice Guideline for the Management of Outpatient Parenteral Antimicrobial Therapy. Clin. Infect. Dis. 2019, 68, e1–e35. [Google Scholar] [CrossRef]
- Gilchrist, M.; Seaton, R.A. Outpatient Parenteral Antimicrobial Therapy and Antimicrobial Stewardship: Challenges and Checklists. J. Antimicrob. Chemother. 2015, 70, 965–970. [Google Scholar] [CrossRef][Green Version]
- Arensdorff, L.; Boillat-Blanco, N.; Decosterd, L.; Buclin, T.; de Vallière, S. Adequate Plasma Drug Concentrations Suggest That Amoxicillin Can Be Administered by Continuous Infusion Using Elastomeric Pumps. J. Antimicrob. Chemother. 2017, 72, 2613–2615. [Google Scholar] [CrossRef]
- Voumard, R.; Gardiol, C.; André, P.; Arensdorff, L.; Cochet, C.; Boillat-Blanco, N.; Decosterd, L.; Buclin, T.; de Vallière, S. Efficacy and Safety of Continuous Infusions with Elastomeric Pumps for Outpatient Parenteral Antimicrobial Therapy (OPAT): An Observational Study. J. Antimicrob. Chemother. 2018, 73, 2540–2545. [Google Scholar] [CrossRef][Green Version]
- Diamantis, S.; Dawudi, Y.; Cassard, B.; Longuet, P.; Lesprit, P.; Gauzit, R. Home Intravenous Antibiotherapy and the Proper Use of Elastomeric Pumps: Systematic Review of the Literature and Proposals for Improved Use. Infect. Dis. Now 2021, 51, 39–49. [Google Scholar] [CrossRef]
- Jenkins, A.; Shanu, S.; Jamieson, C.; Santillo, M. Widening the Net: A Literature Review of Antimicrobial Agents with Potential Suitability for Outpatient Parenteral Antimicrobial Therapy Services-the Importance of Storage and Stability. Eur. J. Hosp. Pharm. Sci. Pract. 2021. [Google Scholar] [CrossRef]
- ASEAN Guidelines on Stability Study of Drug Product. Update Review 22 Février 2005. In Proceedings of the 9th ACCSQ-PPWG Meeting, Manila, Philippines, 21–24 February 2005.
- Guidance for Industry: Drug Stability Guidelines; U.S. Department of Health and Human Services Food and Drug Administration: Silver Spring, MD, USA, 2008.
- Longuet, P.; Lecapitaine, A.L.; Cassard, B.; Batista, R.; Gauzit, R.; Lesprit, P.; Haddad, R.; Vanjak, D.; Diamantis, S.; Groupe des référents en infectiologie d'Île-de-France (GRIF). Preparing and Administering Injectable Antibiotics: How to Avoid Playing God. Med. Mal. Infect. 2016, 46, 242–268. [Google Scholar] [CrossRef]
- Diamantis, S.; Longuet, P.; Lesprit, P.; Gauzit, R. Terms of Use of Outpatient Parenteral Antibiotic Therapy. Infect. Dis. Now 2020, 51, 14–38. [Google Scholar] [CrossRef]
- SFPC (French Society of Clinical Pharmacy) and GERPAC (Evaluation and Research Group on Protection in Controlled Atmospher). SFPC, GERPAC, Methodological Guidelines for Stability Studies of Hospital Pharmaceutical Preparations, Part I: Liquid Preparations. Available online: http://www.gerpac.eu/img/pdf/guide_stabilite_anglais.pdf (accessed on 24 March 2021).
- Allwood, M.C.; Stonkute, D.; Wallace, A.; Wilkinson, A.-S.; Hills, T.; Jamieson, C.; BSAC Drug Stability Working Party. Assessment of the Stability of Citrate-Buffered Flucloxacillin for Injection When Stored in Two Commercially Available Ambulatory Elastomeric Devices: INfusor LV (Baxter) and Accufuser (Woo Young Medical): A Study Compliant with the NHS Yellow Cover Document (YCD) Requirements. Eur. J. Hosp. Pharm. Sci. Pract. 2020, 27, 90–94. [Google Scholar] [CrossRef]
- Souza Barbosa, F.; Capra Pezzi, L.; Tsao, M.; Oliveira, T.F.; Manoela Dias Macedo, S.; Schapoval, E.E.S.; Mendez, A.S.L. Stability and Degradation Products of Imipenem Applying High-Resolution Mass Spectrometry: An Analytical Study Focused on Solutions for Infusion. Biomed. Chromatogr. 2018, 33, e4471. [Google Scholar] [CrossRef]
- Negaban 1 g, Powder for Solution for Injection/Infusio—Summary of Product Characteristics (SmPC)—(Emc). Available online: https://www.medicines.org.uk/emc/product/466 (accessed on 3 March 2021).
- Gorski, L.A. The 2016 Infusion Therapy Standards of Practice. Home Healthc. Now 2017, 35, 10–18. [Google Scholar] [CrossRef]
- Fetcroja 1 g Powder—Summary of Product Characteristics (SmPC)—(Emc). Available online: https://www.medicines.org.uk/emc/product/11771#gref (accessed on 27 January 2022).
- To, T.P.; Ching, M.; Ellis, A.G.; Williams, L.; Garrett, M.K. Stability of Intravenous Flucloxacillin Solutions Used for Hospital-in-the-Home. J. Pharm. Pract. Res. 2010, 40, 101–105. [Google Scholar] [CrossRef]
- Jamieson, C.; Allwood, M.C.; Stonkute, D.; Wallace, A.; Wilkinson, A.-S.; Hills, T.; BSAC Drug Stability Working Party. Investigation of Meropenem Stability after Reconstitution: The Influence of Buffering and Challenges to Meet the NHS Yellow Cover Document Compliance for Continuous Infusions in an Outpatient Setting. Eur. J. Hosp. Pharm. Sci. Pract. 2020, 27, e53–e57. [Google Scholar] [CrossRef]
- Smith, E.K.; McWhinney, B.C. Stability of Buffered Benzylpenicillin and Flucloxacillin for a Paediatric Outpatient Parenteral Antibiotic Therapy Service. J. Pharm. Pract. Res. 2021, 51, 231–237. [Google Scholar] [CrossRef]
- Müller, H.; Haker, I. The Stability of Amoxicillin, Ampicillin, Benzylpenicillin, Flucloxacillin, Mezlocillin and Piperacillin in Isotonic Saline Solutions When Stored in an Innovative Infusion Container (Freeflex Container). Eur. J. Hosp. Pharm. 2003, 9, 106–112. [Google Scholar]
- Trissel, L.A.; Xu, Q.A.; Martinez, J.F. Compatibility and Stability of Aztreonam and Vancomycin Hydrochloride. Am. J. Health-Syst. Pharm. AJHP 1995, 52, 2560–2564. [Google Scholar] [CrossRef] [PubMed]
- Stiles, M.L.; Tu, Y.H.; Allen, L.V. Stability of Cefazolin Sodium, Cefoxitin Sodium, Ceftazidime, and Penicillin G Sodium in Portable Pump Reservoirs. Am. J. Hosp. Pharm. 1989, 46, 1408–1412. [Google Scholar] [CrossRef]
- Loeuille, G.; Vigneron, J.; D'Huart, E.; Charmillon, A.; Demoré, B. Physicochemical Stability of Cefiderocol, a Novel Siderophore Cephalosporin, in Syringes at 62.5 Mg/ML for Continuous Administration in Intensive Care Units. Eur. J. Hosp. Pharm. Sci. Pract. 2021. [Google Scholar] [CrossRef] [PubMed]
- Japanese Pharmacopeia, 17th ed.; Pharmaceuticals and Medical Devices Agency: Tokyo, Japan, 2016; pp. 634–635.
- Abdel-Hamid, M.E. FSQ Spectrophotometric and HPLC Analysis of Some Cephalosporins in the Presence of Their Alkali-Induced Degradation Products. Il Farm. 1998, 53, 132–138. [Google Scholar] [CrossRef]
- Vikram, A.; Prathap, B.; Mallikarjuna, G.; SnehaSowmya, G.; Ushakiranmai, G. Analytical Method Development and Validation for Simultaneous Estimation of Avibactam and Ceftazidime by Rp-Hplc Method. IOSR J. Pharm. 2020, 10, 52–85. [Google Scholar]
- Kratzer, A.; Rothe, U.; Kees, F.; Dorn, C. Stabilität von Ceftolozan/Tazobactam in Infusionslösungen Für Die Verlängerte Oder Kontinuierliche Applikation. Krankenhauspharmazie 2019, 40, 195–200. [Google Scholar]
- Walker, S.E.; Dufour, A.; Iazzetta, J. Concentration and Solution Dependent Stability of Cloxacillin Intravenous Solutions. Can. J. Hosp. Pharm. 1998, 51, 13–19. [Google Scholar] [CrossRef]
- Viaene, E.; Chanteux, H.; Servais, H.; Mingeot-Leclercq, M.-P.; Tulkens, P.M. Comparative Stability Studies of Antipseudomonal Beta-Lactams for Potential Administration through Portable Elastomeric Pumps (Home Therapy for Cystic Fibrosis Patients) and Motor-Operated Syringes (Intensive Care Units). Antimicrob. Agents Chemother. 2002, 46, 2327–2332. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hecq, J.-D.; Berlage, V.; Vanbeckbergen, D.; Jamart, J.; Galanti, L. Effects of Freezing, Long-Term Storage, and Microwave Thawing on the Stability of Piperacillin Plus Tazobactam in 5% Dextrose for Infusion. Can. J. Hosp. Pharm. 2004, 57, 276–282. [Google Scholar] [CrossRef]
- Jamieson, C.; Ozolina, L.; Seaton, R.A.; Gilchrist, M.; Hills, T.; Drummond, F.; Wilkinson, A.S.; BSAC Drug Stability Testing Working Group. Assessment of the Stability of Citrate-Buffered Piperacillin/Tazobactam for Continuous Infusion When Stored in Two Commercially Available Elastomeric Devices for Outpatient Parenteral Antimicrobial Chemotherapy: A Study Compliant with the NHS Yellow Cover Document Requirements. Eur. J. Hosp. Pharm. Sci. Pract. 2020. [Google Scholar] [CrossRef]
- Bird, A.E.; Charsley, C.H.; Jennings, K.R.; Marshall, A.C. High-Performance Liquid Chromatographic Assay of Temocillin and Epimerisation of Its Diastereoisomers. Analyst 1984, 109, 1209–1212. [Google Scholar] [CrossRef]
- Masse, M.; Genay, S.; Carta, N.; Delannoy-Rousselière, C.; Moreau, F.; Faure, K.; Barthélémy, C.; Decaudin, B.; Odou, P. Étude de La Stabilité de La Vancomycine à 40 Mg/ML Au Cours d'une Perfusion de 24 Heures [Poster Presentation]. In Proceedings of the Hopipharm: 65th French Hospital Pharmacy Congress, Nancy, France, 10–12 May 2017. [Google Scholar]
- International Conference on Harmonisation: Validation of Analytical Procedures: Text and Methodology Q2 (R1). Guideline 2005. Available online: http://www.ich.org/fileadmin/public_web_site/ich_products/guidelines/quality/q2_r1/step4/q2_r1__guideline.pdf (accessed on 24 March 2021).
- Bardin, C.; Astier, A.; Vulto, A.; Sewell, G.; Vigneron, J.; Trittler, R.; Daouphars, M.; Paul, M.; Trojniak, M.; Pinguet, F.; et al. Guidelines for the Practical Stability Studies of Anticancer Drugs: A European Consensus Conference. Ann. Pharm. Fr. 2011, 69, 221–231. [Google Scholar] [CrossRef] [PubMed]
- Pharmaceutical Technical Procedures, 2.9.19: Particulate Contamination: Sub-Visible Particles. In European Pharmacopoeia, 10th ed.; European Directorate for the Quality of Medicines and Health Care: Strasbourg, France, 2019; pp. 360–362.
Figure 1. Examples of chromatograms of piperacillin/tazobactam (300/37.5 µg/mL) (A); aztreonam (100 µg/mL) (B); cefotaxime (100 µg/mL) (C); and temocillin R and S (150 µg/mL) (D), obtained immediately after reconstitution in Normal Saline solution.
Figure 1. Examples of chromatograms of piperacillin/tazobactam (300/37.5 µg/mL) (A); aztreonam (100 µg/mL) (B); cefotaxime (100 µg/mL) (C); and temocillin R and S (150 µg/mL) (D), obtained immediately after reconstitution in Normal Saline solution.
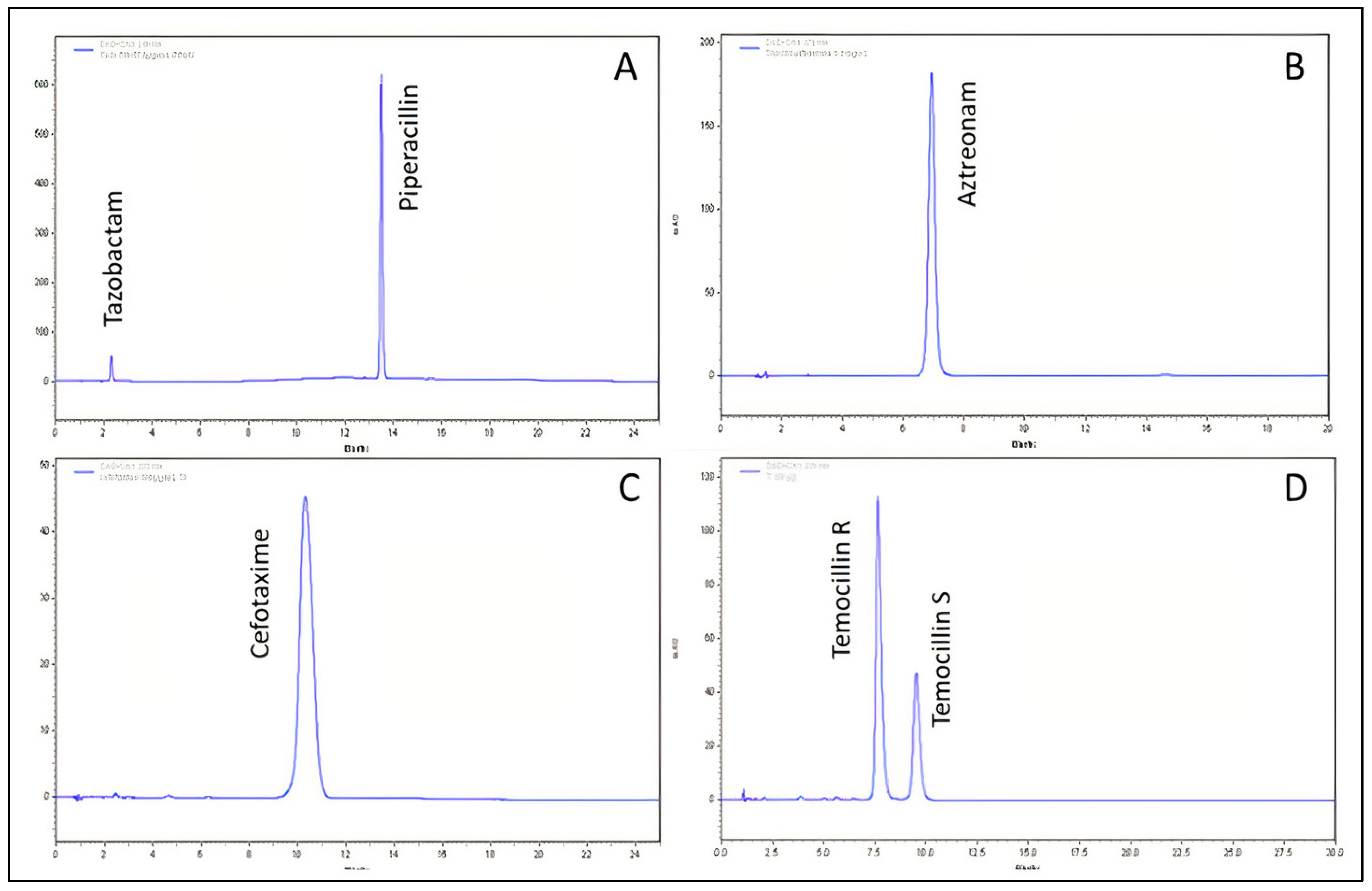
Table 1. Validation criteria for analytical HPLC methods.
Table 1. Validation criteria for analytical HPLC methods.
| Antibiotic | Calibration Range (µg/mL) | R2 | Intra-Day Precision [min; max] (%) | Inter-Day Precision [min; max] (%) | Limit of Detection [µg/mL] | Cochran's Test Cexp | ANOVA (Non-Linearity) Fexp |
|---|---|---|---|---|---|---|---|
| Amoxicillin | 120–280 | 0.9999 | [0.06; 0.66] | [0.57–0.75] | 0.13 | 0.344 | 0.15 |
| Aztreonam | 50–150 | 0.9997 | [0.08; 1.48] | [1.18; 1.95] | 0.51 | 0.399 | 0.93 |
| Cefazolin | 75–175 | 0.9999 | [0.15; 0.85] | [0.44; 0.57] | 0.11 | 0.609 | 0.38 |
| Cefepime | 60–140 | 0.9999 | [0.04; 0.83] | [1.15; 1.70] | 0.36 | 0.269 | 0.13 |
| Cefiderocol | 25–75 | 0.9999 | [0.05; 1.53] | [0.41; 0.99] | 0.10 | 0.424 | 0.07 |
| Cefotaxime | 50–150 | 0.9998 | [0.08; 1.81] | [1.09; 1.66] | 2.02 | 0.600 | 1.93 |
| Cefoxitin | 75–175 | 0.9993 | [0.17; 2.04] | [1.40; 1.80] | 0.53 | 0.420 | 0.66 |
| Ceftazidime | 100–500 | 0.9999 | [0.02; 1.53] | [0.28; 0.94] | 0.23 | 0.533 | 3.06 |
| Ceftazidime/Avibactam | 100–500 | 0.9999 | [0.24; 0.50] | [0.31; 1.05] | 2.43 | 0.551 | 0.21 |
| 25–125 | 0.9999 | [0.13; 0.43] | [0.33; 0.72] | 3.17 | 0.514 | 1.38 | |
| Ceftozolane/Tazobactam | 50–250 | 0.9999 | [0.07; 1.93] | [0.62; 1.47] | 0.77 | 0.579 | 0.26 |
| 25–125 | 0.9999 | [0.06; 2.04] | [0.63; 1.60] | 0.84 | 0.643 | 0.49 | |
| Cloxacillin | 1200–2800 | 0.9981 | [0.33; 1.81] | [1.25; 1;95] | 4.26 | 0.575 | 0.92 |
| Meropenem | 50–250 | 0.9999 | [0.06; 1.30] | [0.71; 1.13] | 0.19 | 0.659 | 0.64 |
| Piperacillin | 100–300 | 0.9999 | [0.01; 0.46] | [0.55; 1.10] | 0.34 | 0.555 | 0.06 |
| Piperacillin/Tazobactam | 100–500 | 0.9999 | [0.12; 1.33] | [0.38; 1.62] | 0.23 | 0.599 | 0.99 |
| 12.5–62.5 | 0.9999 | [0.01; 1.28] | [0.76; 1.44] | 0.36 | 0.554 | 0.14 | |
| Temocillin | 50–250 | 0.9999 | [0.05; 1.72] | [0.91; 2.02] | 0.64 | 0.331 | 0.04 |
| Vancomycin | 50–150 | 0.9995 | [0.03; 1.65] | [1.70; 2.48] | 2.91 | 0.389 | 2.27 |
Table 2. Stability of antibiotics in polypropylene syringes and amoxicillin in polyolefin bags at 20–25 °C for continuous intravenous infusion measured by HPLC.
Table 2. Stability of antibiotics in polypropylene syringes and amoxicillin in polyolefin bags at 20–25 °C for continuous intravenous infusion measured by HPLC.
| Mean % of Initial Concentration ± RSD * % | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Antibiotic | Conc. | Solvent | T0 h | T4 h | T6 h | T8 h | T12 h | T24 h | T48 h |
| Amoxicillin ** | 20 mg/mL | NS | 100 ± 1.19 | - | 96.7 ± 1.77 | - | 94.1 ± 0.66 | 87.5 ± 0.45 | 78.5 ± 1.52 |
| Aztreonam | 125 mg/mL | NS *** | 100.0 ± 2.38 | - | 98.7 ± 0.90 | - | - | 95.3 ± 1.79 | 92.7 ± 1.95 |
| D5W **** | 100.0 ± 0.47 | - | 99.5 ± 0.77 | - | - | 98.1 ± 1.42 | 95.7 ± 0.57 | ||
| Cefazolin | 125 mg/mL | NS | 100.0 ± 2.35 | - | 103.3 ± 1.67 | - | - | 100.0 ± 1.98 | 100.6 ± 1.95 |
| D5W | 100.0 ± 0.91 | - | 99.8 ± 3.11 | - | - | 99.4 ± 1.99 | 97.7 ± 2.10 | ||
| Cefepime | 110 mg/mL | NS | 100.0 ± 2.15 | - | 98.1 ± 0.61 | - | - | 94.8 ± 1.85 | 87.3 ± 0.82 |
| D5W | 100.0 ± 1.78 | - | 94.7 ± 0.93 | - | - | 90.6 ± 0.43 | 85.5 ± 1.80 | ||
| Cefiderocol | 62.5 mg/mL | NS | 100.0 ± 1.30 | - | - | - | 94.2 ± 1.11 | 91.6 ± 0.98 | 85.7 ± 2.24 |
| D5W | 100.0 ± 1.43 | - | - | - | 97.4 ± 0.68 | 94.0 ± 0.73 | 87.1 ± 0.53 | ||
| Cefotaxime | 83.3 mg/mL | NS | 100.0 ± 2.15 | - | 95.3 ± 1.50 | - | 92.2 ± 1.93 | 87.2 ± 2.05 | - |
| D5W | 100.0 ± 1.48 | - | 95.4 ± 1.04 | - | 93.0 ± 1.43 | 88.3 ± 1.45 | - | ||
| 125 mg/mL | NS | 100.0 ± 1.70 | - | 95.7 ± 1.38 | - | 95.2 ± 1.23 | 51.4 ± 1.53 | - | |
| D5W | 100.0 ± 1.21 | - | 97.4 ± 2.00 | - | 94.9 ± 1.18 | - | - | ||
| Cefoxitin | 125 mg/mL | NS | 100.0 ± 1.88 | - | 99.5 ± 0.79 | - | 97.3 ± 3.73 | 94.4 ± 1.60 | 89.8 ± 2.03 |
| D5W | 100.0 ± 1.79 | - | 98.9 ± 1.32 | - | 96.4 ± 3.00 | 93.8 ± 1.80 | 89.6 ± 2.14 | ||
| Ceftazidime | 125 mg/mL | NS | 100.0 ± 0.94 | - | - | 98.3 ± 2.04 | - | 94.9 ± 1.80 | 86.5 ± 1.89 |
| D5W | 100.0 ± 1.69 | - | - | 95.1 ± 1.06 | - | 89.0 ± 0.78 | 82.2 ± 0.44 | ||
| Ceftazidime | 125 mg/mL | NS | 100.0 ± 0.98 | - | - | - | 96.7 ± 0.31 | 95.2 ± 1.33 | 87.4 ± 1.22 |
| D5W | 100.0 ± 1.26 | - | - | - | 98.1 ± 0.86 | 91.7 ± 0.55 | 87.1 ± 1.36 | ||
| Avibactam | 31.25 mg/mL | NS | 100.0 ± 0.86 | - | - | - | 96.4 ± 0.91 | 96.2 ± 1.77 | 91.0 ± 0.89 |
| D5W | 100.0 ± 1.47 | - | - | - | 99.1 ± 0.79 | 94.7 ± 0.77 | 93.0 ± 1.41 | ||
| Ceftozolane | 62.5 mg/mL | NS | 100.0 ± 2.15 | - | - | 96.4 ± 2.25 | - | 93.9 ± 2.25 | 91.8 ± 1.52 |
| D5W | 100.0 ± 1.92 | - | - | 98.5 ± 1.55 | - | 96.2 ± 2.50 | 92.8 ± 0.54 | ||
| Tazobactam | 31.25 mg/mL | NS | 100.0 ± 2.27 | - | - | 98.0 ± 2.57 | - | 99.0 ± 2.30 | 101.0 ± 2.34 |
| D5W | 100.0 ± 2.09 | - | - | 100.0 ± 1.79 | - | 101.3 ± 2.74 | 102.3 ± 0.83 | ||
| Cloxacillin | 250 mg/mL | SWFI ***** | 100.0 ± 1.91 | - | 98.8 ± 1.70 | - | - | 96.2 ± 1.63 | 90.2 ± 1.45 |
| 125 mg/mL | NS | 100.0 ± 3.07 | - | 100.2 ± 1.93 | - | - | 97.2 ± 3.01 | 90.5 ± 2.73 | |
| D5W | 100.0 ± 1.48 | - | 100.0 ± 2.06 | - | - | 97.3 ± 1.47 | 90.1 ± 1.21 | ||
| Meropenem | 41.7 mg/mL | NS | 100.0 ± 1.59 | 97.1 ± 0.66 | - | 93.0 ± 0.93 | - | - | - |
| D5W | 100.0 ± 1.52 | 93.8 ± 0.68 | - | 85.9 ± 0.74 | - | - | - | ||
| Piperacillin | 125 mg/mL | NS | 100.0 ± 0.87 | - | 97.6 ± 0.24 | - | - | 92.8 ± 2.05 | 88.9 ± 1.37 |
| D5W | 100.0 ± 1.11 | - | 100.0 ± 1.97 | - | - | 98.3 ± 1.23 | 97.5 ± 1.26 | ||
| Piperacillin | 125 mg/mL | NS | 100.0 ± 0.96 | - | - | 101.3 ± 0.44 | - | 101 ± 1.26 | 98.1 ± 1.45 |
| D5W | 100.0 ± 2.34 | - | - | 97.1 ± 0.59 | - | 95.9 ± 1.05 | 93.5 ± 0.68 | ||
| Tazobactam | 15.6 mg/mL | NS | 100.0 ± 1.16 | - | - | 100.8 ± 0.40 | - | 101.1 ± 1.56 | 99.4 ± 1.52 |
| D5W | 100.0 ± 2.26 | - | - | 96.3 ± 0.36 | - | 96.7 ± 1.49 | 95.1 ± 1.22 | ||
| Temocillin | Unrealized in syringe | ||||||||
| Vancomycin | 62.5 mg/mL | NS | 100.0 ± 1.65 | - | 99.8 ± 1.17 | - | - | 100.7 ± 1.05 | 99.5 ± 1.27 |
| D5W | 100.0 ± 0.50 | - | 99.3 ± 1.03 | - | - | 98.2 ± 1.34 | 94.6 ± 2.88 | ||
| 83.3 mg/mL | NS | 100.0 ± 1.84 | - | 99.4 ± 1.28 | - | - | 98.4 ± 2.06 | - | |
| D5W | 100.0 ± 1.62 | - | 100.8 ± 0.92 | - | - | 96.0 ± 6.31 | 101.0 ± 0.86 | ||
Table 3. Stability of antibiotics in polyisoprene elastomeric devices for use in OPAT at 37 °C measured by HPLC.
Table 3. Stability of antibiotics in polyisoprene elastomeric devices for use in OPAT at 37 °C measured by HPLC.
| Mean % of Initial Concentration ± RSD * | ||||||||
|---|---|---|---|---|---|---|---|---|
| Antibiotic | Conc. | Solvent NS/D5W | T0 h | T6 h | T8 h | T12 h | T24 h | T48 h |
| Aztreonam | 50 mg/mL | NS ** | 100.0 ± 1.97 | - | - | - | 102.5 ± 3.39 | 100.2 ± 2.17 |
| D5W *** | 100.0 ± 1.64 | - | - | - | 101.7 ± 1.67 | 95.3 ± 2.96 | ||
| Cefazolin | 50 mg/mL | NS | Unstable, precipitate formation during pre-study | |||||
| D5W | ||||||||
| Cefepim | 50 mg/mL | NS | 100.0 ± 1.43 | 93.2 ± 2.00 | - | - | 83.3 ± 2.28 | 59.5 ± 2.21 |
| Cefiderocol | Unrealized in elastomeric device | |||||||
| Cefotaxime | 25 mg/mL | NS | Unstable, colour change after 6 h during pre-study | |||||
| D5W | ||||||||
| Cefoxitine | 25 mg/mL | NS | Unstable, Colour change after 12 h during pre-study | |||||
| D5W | ||||||||
| Ceftazidime | 25 mg/mL | NS | 100.0 ± 3.22 | - | 95.2 ± 1.56 | - | 85.6 ± 2.24 | - |
| D5W | 100.0 ± 2.94 | - | 94.8 ± 3.29 | - | 77.5 ± 1.94 | - | ||
| Ceftazidime | 25 mg/mL | NS | 100.0 ± 3.35 | - | - | 92.2 ± 2.86 | 82.3 ± 2.28 | 66.3 ± 1.90 |
| D5W | 100.0 ± 7.35 | - | - | 86.2 ± 6.54 | 75.4 ± 7.53 | 58.1 ± 8.56 | ||
| Avibactam | 6.25 mg/mL | NS | 100.0 ± 4.59 | - | - | 98.4 ± 4.08 | 96.5 ± 2.95 | 93.9 ± 2.95 |
| D5W | 100.0 ± 7.81 | - | - | 95.4 ± 6.92 | 93.9 ± 7.46 | 90.3 ± 8.35 | ||
| Ceftozolane | 25 mg/mL | NS | 100.0 ± 1.80 | - | 100.0 ± 1.20 | - | 91.8 ± 0.95 | 81.4 ± 3.67 |
| D5W | 100.0 ± 0.99 | - | 97.5 ± 0.85 | - | 89.3 ± 2.11 | 81.7 ± 6.02 | ||
| Tazobactam | 12.5 mg/mL | NS | 100.0 ± 2.08 | - | 104.6 ± 1.47 | - | 109.2 ± 1.33 | 116.7 ± 3.02 |
| D5W | 100.0 ± 0.99 | - | 103.1 ± 0.82 | - | 109.5 ± 1.33 | 116.6 ± 1.83 | ||
| Cloxacillin | 50–100 mg/mL | NS | Unstable, precipitate formation during pre-study | |||||
| D5W | ||||||||
| Meropenem | Unrealized in elastomeric device | |||||||
| Piperacillin | 66.7 mg/mL | NS | Unstable, precipitate formation during pre-study | |||||
| D5W | ||||||||
| Piperacilline | 66.7 mg/mL | NS | 100.0 ± 2.17 | - | 98.5 ± 0.46 | - | 93.6 ± 1.06 | 85.7 ± 1.92 |
| D5W | 100.0 ± 0.74 | - | 97.9 ± 0.87 | - | 93.6 ± 0.60 | 84.1 ± 0.17 | ||
| Tazobactam | 8.3 mg/mL | NS | 100.0 ± 2.26 | - | 98.9 ± 0.53 | - | 97.0 ± 0.93 | 96.2 ± 1.58 |
| D5W | 100.0 ± 0.78 | - | 98.7 ± 0.90 | - | 98.2 ± 0.55 | 95.8 ± 0.25 | ||
| Temocillin | 25 mg/mL | NS | 100.0 ± 2.37 | - | - | - | 92.6 ± 2.95 | 80.4 ± 2.84 |
| D5W | 100.0 ± 2.36 | - | - | - | 87.5 ± 2.23 | 78.8 ± 2.61 | ||
| Vancomycin | 37.5 mg/mL | NS | 100.0 ± 2.06 | - | - | - | 97.9 ± 2.91 | 98.3 ± 3.26 |
| D5W | 100.0 ± 2.70 | - | - | - | 101.0 ± 1.61 | 103.3 ± 1.54 | ||
Table 4. List of antibiotics drugs used for the preparation of solutions.
Table 4. List of antibiotics drugs used for the preparation of solutions.
| Tradename/Manufacturer | Batch Number | |
|---|---|---|
| Amoxicillin | Amoxicilline PANPHARMA 1 g | 307197 |
| Aztreonam | AZACTAM® 1 g SANOFI-AVENTIS | ABC7060 |
| Cefazolin | Céfazoline MYLAN 2 g | 200902–200903 |
| Cefepime | Céfépime MYLAN 2 g | 4M2119FR |
| Cefiderocol | FETCROJA® 1 g SHIONOGI | FEFR0120 |
| Cefotaxime | Céfotaxime MYLAN 2 g | R3052 |
| Cefoxitin | Céfoxitine PANPHARMA 2 g | N4-03 |
| Ceftazidime | Ceftazidime MYLAN 2 g | 191102 |
| Ceftazidime/Avibactam | ZAVICEFTA® 2/0.5 g PFIZER | 3M05L95690 |
| Ceftozolane/Tazobactam | ZERBAXA® 1/0.5 g MERCK SHARP & DOHME BV | T003341 |
| Cloxacillin | ORBENINE® 1 g ASTELLAS | 25AND02/ 25AQF03 |
| Meropenem | Méropénem PANPHARMA 1 g | MFR1020 |
| Piperacillin | Pipéracilline PANPHARMA 4 g Pipéracilline PANPHARMA 1 g | 306609–306699 306421 |
| Piperacillin/Tazobactam | Pipéracilline/tazobactam PANPHARMA 4/0.5 g | 306584 |
| Temocillin | NEGABAN® 1 g EUMEDICA NEGABAN® 2 g | L154510 L162439 |
| Vancomycin | Vancomycine SANDOZ 1 g | EC0107 |
Table 5. Preparation of test solutions.
Table 5. Preparation of test solutions.
| Antibiotic | Polyolefin Bag (100 mL, 20–25 °C) | Syringe (48 mL, 20–25 °C) | Elastomeric Device (37 °C) | |||
|---|---|---|---|---|---|---|
| Amount (g) | Solvent | Amount (g) | Solvent | Amount (g) | Solvent | |
| (Concentration mg/mL) | (Concentration mg/mL) | (Concentration mg/mL) | ||||
| Amoxicillin | 2 g 20 mg/mL | NS * | Unrealized | |||
| Aztreonam | Unrealized | 6 g (125 mg/mL) | NS—D5W ** | 6 g (120 mL) (50 mg/mL) | NS—D5W | |
| Cefazolin | Unrealized | 6 g (125 mg/mL) | NS—D5W | 6 g (120 mL) (50 mg/mL) | NS—D5W | |
| Cefepime | Unrealized | 6 g (125 mg/mL) | NS—D5W | 6 g (120 mL) (50 mg/mL) | NS | |
| Cefiderocol | Unrealized | 3 g (62.5 mg/mL) | NS—D5W | 6 g (240 mL) (25 mg/mL) | NS—D5W | |
| Cefotaxime | Unrealized | 4 g (83.3 mg/mL) | NS—D5W | 6 g (240 mL) (25 mg/mL) | NS—D5W | |
| 6 g (125 mg/mL) | NS—D5W | |||||
| Cefoxitin | Unrealized | 6 g (125 mg/mL) | NS—D5W | 6 g (240 mL) (25 mg/mL) | NS—D5W | |
| Ceftazidime | Unrealized | 6 g (125 mg/mL) | NS—D5W | 3 g (120 mL) (25 mg/mL) | NS—D5W | |
| Ceftazidime/Avibactam | Unrealized | 6/1.5 g (125/31.25 mg/mL) | NS—D5W | 3/0.75 g (120 mL) (25/6.25 mg/mL) | NS- D5W | |
| Ceftozolane/Tazobactam | Unrealized | 3/1.5 g (62.5/31.25 mg/mL) | NS—D5W | 3/1.5 g (120 mL) (25/12.5 mg/mL) | NS—D5W | |
| Cloxacillin | Unrealized | 12 g (250 mg/mL) | SWFI *** | 12 g (120 mL) (100 mg/mL) 12 g (240 mL) (50 mg/mL) | NS—D5W | |
| 6 g (125 mg/mL) | NS—D5W | |||||
| Meropenem | Unrealized | 2 g (41.7 mg/mL) | NS—D5W | Unrealized | ||
| Piperacillin | Unrealized | 6 g (125 mg/mL) | NS—D5W | 16 g (240 mL) (66.7 mg/mL) | NS—D5W | |
| Piperacillin/Tazobactam | Unrealized | 6/0.75 g (125/15.6 mg/mL) | NS—D5W | 16 g/2 (240 mL) (66.7/8.3 mg/mL) | NS—D5W | |
| Temocillin | Unrealized | Unrealized 1 | 6 g (240 mL) (25 mg/mL) | NS—D5W | ||
| Vancomycin | Unrealized | 3 g (62.5 mg/mL) | NS—D5W | 4.5 g (120 mL) (37.5 mg/mL) | NS—D5W | |
| Unrealized | 4 g (83.3 mg/mL) | |||||
Table 6. List of HPLC conditions for the antibiotic stability studies.
Table 6. List of HPLC conditions for the antibiotic stability studies.
| Antibiotic | Mobile Phase (v/v) | pH | Flow Rate (mL/min) | Injection Volume (µL) | Wavelength (nm) | Retention Time (min) | Reference |
|---|---|---|---|---|---|---|---|
| Amoxicillin | Isocratic: NaH2PO4 buffer 0.05 M/methanol (95/5) | 4.4 | 1.0 | 50 | 220 | 4.45 | [26] |
| Aztreonam | Isocratic: KH2PO4 buffer 0.05 M/methanol (90/10) | 3.0 | 1.0 | 20 | 270 | 6.9 | [27] |
| Cefazolin | Isocratic: KH2PO4 buffer 0.005 M/methanol (80/20) | 7.5 | 1.0 | 50 | 272 | 3.0 | [28] |
| Cefepime | Isocratic: KH2PO4 buffer 0.005 M/methanol (90/10) | 7.5 | 1.0 | 50 | 257 | 3.8 | [28] |
| Cefiderocol | Gradient: KH2PO4 buffer 0.05 M (A) + methanol (B) T0 to T7 min gradual increase 83/17 (A/B) to 70/30; T7 to T15 min: 70/30; T16 to T20 min: 83/17 | 3.0 | 1.5 | 50 | 260 | 5.9 | [29] |
| Cefotaxime | Gradient: Na2HPO4 buffer 0.05 M/methanol (86/14) (A); Na2HPO4 buffer 0.05 M/methanol (60/40) (B) T0 to T7 min: 100/0 (A/B); T9 to T16 min: 80/20; T16 to T30 min: gradual increase until 41.4/58.6; T35 to T40 min: 100/0 | 6.25 | 1.3 | 10 | 235 | 9.0 | [30] |
| Cefoxitin | Isocratic: KH2PO4 buffer 0.005 M/methanol (80/20) | 7.5 | 1.0 | 10 | 272 | 3.2 | [28] |
| Ceftazidime | Isocratic: ammonium acetate 0.1 M/acetonitrile 90/10 | 7.5 | 1.0 | 20 | 260 | 4.1 | [31] |
| Ceftazidime/Avibactam | Gradient: KH2PO4 buffer 0.05 M (A) + methanol (B) T0 to T4 min: 99/1 (A/B); T9 to T28 min: 90/10; T36 to T40 min: 99/1 | 3 | 1.5 | 20 | 260 | 20.3/1.6 | [32] |
| Ceftozolane/Tazobactam | Isocratic: KH2PO4 buffer 0.005 M/acetonitrile (1000/26) | 3.4 | 1.0 | 20 | 220 | 8.7/4.8 | [33] |
| Cloxacillin | Isocratic: triethylamine + tetrabutylammonium buffer/methanol (35/65) | 6 | 0.5 | 5 | 250 | 4.5 | [34] |
| Meropenem | Isocratic: ammonium acetate 10.53 mM /acetonitrile (95/5) | 3.0 | 1.0 | 20 | 297 | 8.1 | [35] |
| Piperacillin | Isocratic: KH2PO4 buffer 0.05 M/acetonitrile (55/45) | 3.0 | 1.0 | 2 | 230 | 3.4 | [36] |
| Piperacillin/Tazobactam | Gradient: KH2PO4 0.02 M (A)/acetonitrile (B) T0 to T5 min: 92.5/7.5 (A/B); T10 to T15 min: 70/30; T20 to T25 min: 92.5/7.5 | 2.5 | 1.5 | 10 | 210/280 | 13.5/ | [37] |
| 2.2 | |||||||
| Temocillin | Isocratic: KH2PO4 buffer 0.1 M/methanol (93/7) | 7.0 | 1.0 | 20 | 230 | 7.6 and 9.2 | [38] |
| Vancomycin | Isocratic: KH2PO4 buffer 0.1 M/acetonitrile (92/8) | 3.5 | 1.5 | 10 | 220 | 7.2 | [39] |
Table 7. Stability data for antibiotics in syringes, polyolefin bags *, or elastomeric devices.
Table 7. Stability data for antibiotics in syringes, polyolefin bags *, or elastomeric devices.
| Antibiotic | Syringe (48 mL, 25 °C), Polyolefin Bags * (100 mL, 25 °C) | Diffuser (37 °C) | ||||
|---|---|---|---|---|---|---|
| Amount (g) | Solvent | Stability (Hours) | Amount (g) | Solvent | Stability (Hours) | |
| (Concentration) | (Concentration) | |||||
| Amoxicillin * | 2 g (100 mL) (20 mg/mL) | NS ** | 12 h | Unrealized in elastomeric device | ||
| Aztreonam | 6 g | NS-D5W *** | 48 h | 6 g (120 mL) (50 mg/mL) | NS-D5W | 48 h |
| (125 mg/mL) | ||||||
| Cefazolin | 6 g | NS-D5W | 24 h | 6 g (120 mL) (50 mg/mL) | NS-D5W | Precipitate formation during the pre-study |
| (125 mg/mL) | ||||||
| Cefepime | 6 g | NS-D5W | 24 h | 6 g (120 mL) (50 mg/mL) | NS | Visual modification after 6 h at 37 °C |
| (125 mg/mL) | ||||||
| Cefiderocol | 3 g | NS-D5W | 24 h | 6 g (240 mL) (25 mg/mL) | NS- D5W | 6 h |
| (62.5 mg/mL) | ||||||
| Cefotaxime | 4 g–6 g | NS-D5W | 6 h | 6 g (240 mL) (25 mg/mL) | NS-D5W | Colour change after 6 h during the pre-study |
| (83.3–125 mg/mL) | ||||||
| Cefoxitin | 6 g | D5W | 12 h | 6 g (240 mL) (25 mg/mL) | NS-D5W | Instability during the pre-study |
| (125 mg/mL) | ||||||
| Ceftazidime | 6 g | NS | 24 h | 3 g (120 mL) (25 mg/mL) | NS-D5W | 8 h |
| (125 mg/mL) | D5W | 8 h | ||||
| Ceftazidime/ | 6/1.5 g | NS-D5W | 24 h | 3/0.75 g (120 mL) | NS | 12 h |
| Avibactam | (125/31.25 mg/mL) | (25/6.25 mg/mL) | D5W | Unstable | ||
| Ceftozolane/ | 3/1.5 g | NS-D5W | 48 h | 3/1.5 g (120 mL) | NS D5W | 12 h 8 h |
| Tazobactam | (62.5/31.25 mg/mL) | (25/12.5 mg/mL) | ||||
| Cloxacillin | 12 g | SWFI **** | 24 h | 6–12 g (120 mL) (50–100 mg/mL) | NS-D5W | Precipitate formation during the pre-study |
| (250 mg/mL) | ||||||
| 6 g | NS-D5W | 24 h | ||||
| (125 mg/mL) | ||||||
| Meropenem | 2 g | NS | 8 h | Unrealized in elastomeric device | ||
| (41.7 mg/mL) | D5W | 4 h | ||||
| Piperacillin | 6 g | NS | 24 h | 16 g (240 mL) (66.7 mg/mL) | NS-D5W | Instability during the pre-study |
| (125 mg/mL) | D5W | 48 h | ||||
| Piperacillin / | 6/0.75 g | NS-D5W | 48 h | 16/2 g (240 mL) | NS | 8 h |
| Tazobactam | (125/15.6 mg/mL) | (66.7/8.3 mg/mL) | D5W | 24 h | ||
| Temocillin | Unrealized | 6 g (240 mL) | NS | 24 h | ||
| (25 mg/mL) | D5W | Unstable | ||||
| Vancomycin | 3 g | D5W | 48 h | 4,5 g (120 mL) (37.5 mg/mL) | NS-D5W | 48 h |
| (62.5 mg/mL) | ||||||
| 4 g | D5W | 48 h | ||||
| (83.3 mg/mL) | ||||||
| Publisher's Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Source: https://www.mdpi.com/2079-6382/11/4/458/htm
0 Response to "Continuous Vs Discontinuous Therapy With Penicillin"
Post a Comment